DISCUSSION
A. DISINFECTANTS, ANTISEPTICS, AND SANITIZERS
Disinfection is the elimination of microorganisms, but not necessarily endospores, from inanimate objects or surfaces, whereas decontamination is the treatment of an object or inanimate surface to make it safe to handle.
a. The term disinfectant is used for an agent used to disinfect inanimate objects or surfaces but is generally to toxic to use on human tissues.
b. The term antiseptic refers to an agent that kills or inhibits growth of microbes but is safe to use on human tissue.
c. The term sanitizer describes an agent that reduces, but may not eliminate, microbial numbers to a safe level.
Because disinfectants and antiseptics often work slowly on some viruses - such as the hepatitis viruses, bacteria with an acid-fast cell wall such as Mycobacterium tuberculosis, and especially bacterial endospores, produced by the genus Bacillus and the genus Clostridium, they are usually unreliable for sterilization - the destruction of all life forms.
There are a number of factors which influence the antimicrobial action of disinfectants and antiseptics, including:
1. The concentration of the chemical agent.
2. The temperature at which the agent is being used. Generally, the lower the temperature, the longer it takes to disinfect or decontaminate.
3. The kinds of microorganisms present. Endospore producers such as Bacillus species, Clostridium species, and acid-fast bacteria like Mycobacterium tuberculosis are harder to eliminate.
4. The number of microorganisms present. The more microorganisms present, the harder it is to disinfect or decontaminate.
5. The nature of the material bearing the microorganisms. Organic material such as dirt and excreta interferes with some agents.
The best results are generally obtained when the initial microbial numbers are low and when the surface to be disinfected is clean and free of possible interfering substances.
There are 2 common antimicrobial modes of action for disinfectants, antiseptics, and sanitizers:
1. They may damage the lipids and/or proteins of the semipermeable cytoplasmic membrane of microorganisms resulting in leakage of cellular materials needed to sustain life.
2. They may denature microbial enzymes and other proteins, usually by disrupting the hydrogen and disulfide bonds that give the protein its three-dimensional functional shape. This blocks metabolism.
A large number of such chemical
agents are in common use. Some of the more common groups are listed below:
1. Phenol and phenol derivatives Phenol (5-10%) was the first disinfectant commonly used. However, because of its toxicity and odor, phenol derivatives (phenolics) are now generally used. The most common phenolic is orthophenylphenol, the agent found in O-syl®, Staphene®, and Amphyl®. Bisphenols contain two phenolic groups and typically have chlorine as a part of their structure. They include hexachlorophene and triclosan. Hexachlorophene in a 3% solution is combined with detergent and is found in PhisoHex®. Triclosan is an antiseptic very common in antimicrobial soaps and other products. Biguanides include chlorhexadine and alexidine. A 4% solution of chlorhexidine in isopropyl alcohol and combined with detergent (Hibiclens® and Hibitane®) is a common hand washing agent and surgical handscrub. These agents kill most bacteria, most fungi, and some viruses, but are usually ineffective against endospores. Chloroxylenol (4-chloro-3,5-dimethylphenol) is a broad spectrum antimicrobial chemical compound used to control bacteria, algae, fungi and virus and is often used in antimicrobial soaps and antiseptics. Phenol and phenolics alter membrane permeability and denature proteins. Bisphenols, biguanides, and chloroxylenol alter membrane permeability. 2. Soaps and detergents Soaps are only mildly microbicidal. Their use aids in the mechanical removal of microorganisms by breaking up the oily film on the skin (emulsification) and reducing the surface tension of water so it spreads and penetrates more readily. Some cosmetic soaps contain added antiseptics to increase antimicrobial activity. Detergents may be anionic or cationic. Anionic (negatively charged) detergents, such as laundry powders, mechanically remove microorganisms and other materials but are not very microbicidal. Cationic (positively charged) detergents alter membrane permeability and denature proteins. They are effective against many vegetative bacteria, some fungi, and some viruses. However, bacterial endospores and certain bacteria such as Mycobacterium tuberculosisand Pseudomonas species are usually resistant. Soaps and organic materials like excreta also inactivate them. Cationic detergents include the quaternary ammonium compounds such as benzalkonium chloride, zephiran®, diaprene, roccal, ceepryn, and phemerol. Household Lysol® contains alkyl dimethyl benzyl ammonium chloride and alcohols. 3. Alcohols 70% solutions of ethyl or isopropyl alcohol are effective in killing vegetative bacteria, enveloped viruses, and fungi. However, they are usually ineffective against endospores and non-enveloped viruses. Once they evaporate, their cidal activity will cease. Alcohols denature membranes and proteins and are often combined with other disinfectants, such as iodine, mercurials, and cationic detergents for increased effectiveness. 4. Acids and alkalies Acids and alkalies alter membrane permeability and denature proteins and other molecules. Salts of organic acids, such as calcium propionate, potassium sorbate, and methylparaben, are commonly used as food preservatives. Undecylenic acid (Desenex®) is used for dermatophyte infections of the skin. An example of an alkali is lye (sodium hydroxide).
5. Heavy metals Heavy metals, such as mercury, silver, and copper, denature proteins. Mercury compounds (mercurochrome, metaphen, merthiolate) are only bacteriostatic and are not effective against endospores. Silver nitrate (1%) is sometimes put in the eyes of newborns to prevent gonococcal ophthalmia. Copper sulfate is used to combat fungal diseases of plants and is also a common algicide. Selinium sulfide kills fungi and their spores. 6. Chlorine Chlorine gas reacts with water to form hypochlorite ions, which in turn denature microbial enzymes. Chlorine is used in the chlorination of drinking water, swimming pools, and sewage. Sodium hypochlorite is the active agent in household bleach. Calcium hypochlorite, sodium hypochlorite, and chloramines (chlorine plus ammonia) are used to sanitize glassware, eating utensils, dairy and food processing equipment, hemodialysis systems, and treating water supplies. 7. Iodine and iodophores Iodine also denatures microbial proteins. Iodine tincture contains a 2% solution of iodine and sodium iodide in 70% alcohol. Aqueous iodine solutions containing 2% iodine and 2.4% sodium iodide are commonly used as a topical antiseptic. Iodophores are a combination of iodine and an inert polymer such as polyvinylpyrrolidone that reduces surface tension and slowly releases the iodine. Iodophores are less irritating than iodine and do not stain.They are generally effective against vegetative bacteria, Mycobacterium tuberculosis, fungi, some viruses, and some endospores. Examples include Wescodyne®, Ioprep®, Ioclide®, Betadine®, and Isodine®. 8. Aldehydes Aldehydes, such as formaldehyde and glutaraldehyde, denature microbial proteins. Formalin (37% aqueous solution of formaldehyde gas) is extremely active and kills most forms of microbial life. It is used in embalming, preserving biological specimens, and in preparing vaccines. Alkaline glutaraldehyde (Cidex®), acid glutaraldehyde (Sonacide®), and glutaraldehyde phenate solutions (Sporocidin®) kill vegetative bacteria in 10-30 minutes and endospores in about 4 hours. A 10 hour exposure to a 2% glutaraldehyde solution can be used for cold sterilization of materials. Ortho-phthalaldehyde (OPA) is dialdehyde used as a high-level disinfectant for medical instruments. 9. Peroxygens Peroxygens are oxidizing agentes that include hydrogen peroxide and peracetic acid. Hydrogen peroxide is broken down into water and oxygen by the enzyme catalase in human cells and is not that good of an antiseptic for open wounds but is useful for disinfecting inanimate objects. The high concentrations of hydrogen peroxide overwhelm the catalase found in microbes. Peracetic acid is a disinfectant that kills microorganisms by oxidation and subsequent disruption of their cytoplasmic membrane. It is widely used in healthcare, food processing, and water treatment. 10. Ethylene oxide gas Ethylene oxide is one of the very few chemicals that can be relied upon for sterilization (after 4-12 hours exposure). Since it is explosive, it is usually mixed with inert gases such as freon or carbon dioxide. Gaseous chemosterilizers, using ethylene oxide, are commonly used to sterilize heat-sensitive items such as plastic syringes, petri plates, textiles, sutures, artificial heart valves, heart-lung machines, and mattresses. Ethylene oxide has very high penetrating power and denatures microbial proteins. Vapors are toxic to the skin, eyes, and mucous membranes and are also carcinogenic. Another gas that is used as a sterilant is chlorine dioxide which denatures proteins in vegetative bacteria, bacterial endospores, viruses, and fungi.
B. EVALUATION OF DISINFECTANTS, ANTISEPTICS, AND SANITIZERS
It is possible to evaluate disinfectants, antiseptics, and sanitizers using either in vitro or in vivo tests. An in vitro test is one done under artificial, controlled laboratory conditions. An in vivo test is one done under the actual conditions of normal use.
A common in vitro test is to compare the antimicrobial activity of the agent being tested with that of phenol. The resulting value is called a phenol coefficient and has some value in comparing the strength of disinfectants under standard conditions. Phenol coefficients may be misleading, however, because as mentioned earlier, the killing rate varies greatly with the conditions under which the chemical agents are used. The concentration of the agent, the temperature at which it is being used, the length of exposure to the agent, the number and kinds of microorganisms present, and the nature of the material bearing the microorganisms all influence the antimicrobial activity of a disinfectant. If a disinfectant is being evaluated for possible use in a given in vivo situation, it must be evaluated under the same conditions in which it will be used.
C. EFFECTIVENESS OF HAND WASHING
There are 2 categories of microorganisms, or flora, normally found on the hands. Resident flora are the normal microbiota of the skin. Transient flora are the microorganisms you pick up from what you have been handling. It is routine practice to wash the hands prior to and after examining a patient and to do a complete regimented surgical scrub prior to going into the operating room. This is done in order to remove the potentially harmful transient flora, reduce the number of resident flora, and disinfect the skin.
Actual sterilization of the hands is not possible since microorganisms live not only on the surface of the skin but also in deeper skin layers, in ducts of sweat glands, and around hair follicles. These normal microbiota are mainly nonpathogenic staphylococci (Lab 15) and diphtheroid bacilli.
D. ANTIMICROBIAL CHEMOTHERAPEUTIC AGENTS
Antimicrobial chemotherapy is the use of chemicals to inhibit or kill microorganisms in or on the host. Chemotherapy is based on selective toxicity. This means that the agent used must inhibit or kill the microorganism in question without seriously harming the host.
In order to be selectively toxic, a chemotherapeutic agent must interact with some microbial function or microbial structure that is either not present or is substantially different from that of the host. For example, in treating infections caused by prokaryotic bacteria, the agent may inhibit peptidoglycan synthesis or alter bacterial (prokaryotic) ribosomes. Human cells do not contain peptidoglycan and possess eukaryotic ribosomes. Therefore, the drug shows little if any effect on the host (selective toxicity). Eukaryotic microorganisms, on the other hand, have structures and functions more closely related to those of the host. As a result, the variety of agents selectively effective against eukaryotic microorganisms such as fungi and protozoans is small when compared to the number available against prokaryotes. Also keep in mind that viruses are not cells and, therefore, lack the structures and functions altered by antibiotics so antibiotics are not effective against viruses.
Based on their origin, there are 2 general classes of antimicrobial chemotherapeutic agents:
1. antibiotics: substances produced as metabolic products of one microorganism which inhibit or kill other microorganisms.
2. antimicrobial chemotherapeutic chemicals: chemicals synthesized in the laboratory which can be used therapeutically on microorganisms.
Today the distinction between the 2 classes is not as clear, since many antibiotics are extensively modified in the laboratory (semisynthetic) or even synthesized without the help of microorganisms.
Most of the major groups of antibiotics were discovered prior to 1955, and most antibiotic advances since then have come about by modifying the older forms. In fact, only 3 major groups of microorganisms have yielded useful antibiotics: the actinomycetes (filamentous, branching soil bacteria such as Streptomyces), bacteria of the genus Bacillus, and the saprophytic molds Penicillium and Cephalosporium.
To produce antibiotics, manufacturers inoculate large quantities of medium with carefully selected strains of the appropriate species of antibiotic-producing microorganism. After incubation, the drug is extracted from the medium and purified. Its activity is standardized and it is put into a form suitable for administration.
Some antimicrobial agents are cidal in action: they kill microorganisms (e.g., penicillins, cephalosporins, streptomycin, neomycin). Others are static in action: they inhibit microbial growth long enough for the body's own defenses to remove the organisms (e.g., tetracyclines, erythromycin, sulfonamides).
Antimicrobial agents also vary in their spectrum. Drugs that are effective against a variety of both Gram-positive and Gram-negative bacteria are said to be broad spectrum (e.g., tetracycline, streptomycin, cephalosporins, ampicillin, sulfonamides). Those effective against just Gram-positive bacteria, just Gram negative bacteria, or only a few species are termed narrow spectrum (e.g., penicillin G, erythromycin, clindamycin, gentamicin).
If a choice is available, a narrow spectrum is preferable since it will cause less destruction to the body's normal flora. In fact, indiscriminate use of broad spectrum antibiotics can lead to superinfection by opportunistic microorganisms, such as Candida (yeast infections) and Clostridium difficile (antibiotic-associated ulcerative colitis), when the body's normal flora is destroyed. Other dangers from indiscriminate use of antimicrobial chemotherapeutic agents include drug toxicity, allergic reactions to the drug, and selection for resistant strains of microorganisms.
Below are examples of commonly used antimicrobial chemotherapeutic agents arranged according to their mode of action:
1. Antimicrobial agents that inhibit peptidoglycan synthesis. Inhibition of peptidoglycan synthesis in actively-dividing bacteria results in osmotic lysis. (A list of common antimicrobial chemotherapeutic agents listed by both their generic and brand names and arranged by their mode of action can be found in Table 1.)
a. Penicillins (produced by the mold Penicillium)
There are several classes of penicillins:
1. Natural penicillins are highly effective against Gram-positive bacteria (and a very few Gram-negative bacteria) but are inactivated by the bacterial enzyme penicillinase. Examples include penicillin G, F, X, K, O, and V.
2. Semisynthetic penicillins are effective against Gram-positive bacteria but are not inactivated by penicillinase. Examples include methicillin, dicloxacillin, and nafcillin.
3. Semisynthetic broad-spectrum penicillins are effective against a variety of Gram-positive and Gram-negative bacteria but are inactivated by penicillinase. Examples include ampicillin, carbenicillin, oxacillin, azlocillin, mezlocillin, and piperacillin.
4. Semisynthetic broad-spectrum penicillins combined with beta lactamase inhibitors such as clavulanic acid and sulbactam. Although the clavulanic acid and sulbactam have no antimicrobial action of their own, they inhibits penicillinase thus protecting the penicillin from degradation. Examples include amoxicillin plus clavulanic acid, ticarcillin plus clavulanic acid, and ampicillin plus sulbactam.
b. Cephalosporins (produced by the mold Cephalosporium)
Cephalosporins are effective against a variety of Gram-positive and Gram-negative bacteria and are resistant to penicillinase (although some can be inactivated by other beta-lactamase enzymes similar to penicillinase). Four "generations" of cephalosporins have been developed over the years in an attempt to counter bacterial resistance.
1. First generation cephalosporins include cephalothin, cephapirin, and cephalexin.
2. Second generation cephalosporins include cefamandole, cefaclor, cefazolin, cefuroxime, and cefoxitin.
3. Third generation cephalosporins include cefotaxime, cefsulodin, cefetamet, cefixime, ceftriaxone, cefoperazone, ceftazidine, and moxalactam.
4. Fourth generation cephalosporins include cefepime and cefpirome.
c. Carbapenems: Carbapenems consist of a broad spectrum beta lactam antibiotic to inhibit peptidoglycan synthesis combined with cilastatin sodium, an agent which prevents degradation of the antibiotic in the kidneys. Examples include: imipenem, metropenem, ertapenem, and doripenem.
d. Monobactems: Monobactems are broad spectrum beta lactam antibiotics resistant to beta lactamase. An example is aztreonam.
e. Carbacephem: A synthetic cephalosporins. An example is loracarbef.
e. Glycopeptides (produced by the bacterium Streptomyces): Vancomycin and teichoplanin are glycopeptides that are effective against Gram-positive bacteria.
f. Bacitracin (produced by the bacterium Bacillus): Bacitracin is used topically against Gram-positive bacteria.
h. Fosfomycin (Monurol )
2. A few antimicrobial chemotherapeutic agents inhibit normal synthesis of the acid-fast cell wall of the genus Mycobacterium.
a. INH (isoniazid) appears to block the synthesis of mycolic acid, a key component of the acid-fast cell wall of mycobacteria.
b. Ethambutol interferes with the synthesis of the outer membrane of acid-fast cell walls.3. Antimicrobial agents that alter the cytoplasmic membrane. Alteration of the cytoplasmic membrane of microorganisms results in leakage of cellular materials. (A list of common antimicrobial chemotherapeutic agents listed by both their generic and brand names and arranged by their mode of action can be found in Table 1.)
a. Polymyxins and colistins act as detergents and alter membrane permeability in Gram-negative bacteria. They cannot effectively diffuse through the thick peptidoglycan layer in Gram-positives.
b. Daptomycin disrupts the bacterial cytoplasmic membrane function by apparently binding to the membrane and causing rapid depolarization. This results on a loss of membrane potential and leads to inhibition of protein, DNA and RNA synthesis, resulting in bacterial cell death.
c. Pyrazinamide inhibits fatty acid synthesis in the membranes of Mycobacterium tuberculosis.
d. Amphotericin B, produced by the bacterium Streptomyces, is used for systemic fungal infections. It interferes with membrane permeability by interacting with membrane sterols called ergosterols and forming pores in the membrane causing cellular leakage.
e. Nystatin, produced by the bacterium Streptomyces, is used mainly for Candida yeast infections. It interferes with membrane permeability by interacting with membrane sterols called ergosterols and forming pores in the membrane causing cellular leakage.
f. Imidazoles, produced by the bacterium Streptomyces, are antifungal antibiotics used for yeast infections, dermatophytic infections, and systemic fungal infections. They interfere with the synthesis of ergosterol, the sterol in fungal cytoplasmic membranes, causing cellular leakage. Examples include clotrimazole, miconazole, ketoconazole, itraconazole, and fluconazole.
4. Antimicrobial agents that inhibit protein synthesis. (A list of common antimicrobial chemotherapeutic agents listed by both their generic and brand names and arranged by their mode of action can be found in Table 1.)
These agents prevent bacteria from synthesizing structural proteins and enzymes.
a. Agents that block transcription (prevent the synthesis of mRNA off of DNA).
Rifampin or Rifampicin: rifadin, rifater combined with isoniazid and pyrazinamide , rimactane (produced by the bacterium Streptomyces). Rifaximins are effective against some Gram‑positive and Gram-negative bacteria and Mycobacterium tuberculosis.
b. Agents that block translation (alter bacterial ribosomes to prevent mRNA from being translated into proteins).
1. The aminoglycosides (streptomycin, neomycin, netilmicin, tobramycin, gentamicin, amikacin, etc.) bind irreversibly to the 16S rRNA in the 30S subunit of bacterial ribosomes interfering with the translation stage of protein syntheses. Although the exact mechanism of action is still uncertain, there is evidence that some prevent the transfer of the peptidyl tRNA from the A-site to the P-site, thus preventing the elongation of the polypeptide chain. Some aminoglycosides also appear to interfere with the proofreading process that helps assure the accuracy of translation. Possibly the antibiotics reduce the rejection rate for tRNAs that are near matches for the codon. This leads to misreading of the codons or premature termination of protein synthesis. Aminoglycosides may also interfere directly or indirectly with the function of the bacterial cytoplasmic membrane. Because of their toxicity, aminoglycosides are generally used only when other first line antibiotics are not effective.
2. The tetracyclines (tetracycline, doxycycline, demeclocycline, minocycline, etc.) bind reversibly to the 16S rRNA in the 30S ribosomal subunit interfering with the translation stage of protein synthese. They distort the ribosome in such a way that the anticodons of charged tRNAs cannot align properly with the codons of the mRNA Examples include tetracycline, minocycline, and doxycycline, produced by the bacterium Streptomyces. They are effective against a variety of Gram-positive and Gram-negative bacteria.
3. Lincomycin and clindamycin, produced by the bacterium Streptomyces, bind reversibly to the 23S rRNA in the 50s ribosomal subunit and block peptide bond formation during the translation stage of protein synthesis. Most are used against Gram-positive bacteria.
4. The macrolides (erythromycin, azithromycin, clarithromycin, dirithromycin, troleandomycin, etc.) bind reversibly to the 23S rRNA in the 50S subunit of bacterial ribosomes interfering with the translation stage of protein syntheses. They appear to inhibit elongation of the protein by preventing the enzyme peptidyltransferase from forming peptide bonds between the amino acids. They may also prevent the transfer of the peptidyl tRNA from the A-site to the P-site as the beginning peptide chain on the peptidyl tRNA adheres to the ribosome, creates friction, and blocks the exit tunnel of the 50S ribosomal subunit. Macrolides are used against Gram-positive bacteria and some Gram-negative bacteria.
5. The oxazolidinones (linezolid), following the first cycle of protein synthesis, interfere with translation sometime before the initiation phase. They appear to bind to the 50S ribosomal subunit and interfere with its binding to the initiation complex.
6. The streptoGramins (synercid, a combination of quinupristin and dalfopristin) bind to two different locations on the 23S rRNA in the 50S ribosomal subunit and work synergistically to block the translation stage of protein synthesis. There are reports that the streptoGramins may inhibit the attachment of the charged tRNA to the A-site or may block the peptide exit tunnel of the 50S ribosomal subunit.
5. Antimicrobial agents that interfere with DNA synthesis. (A list of common antimicrobial chemotherapeutic agents listed by both their generic and brand names and arranged by their mode of action can be found in Table 1.)
a.The fluoroquinolones (norfloxacin, lomefloxacin, fleroxacin, ciprofloxacin, enoxacin, trovafloxacin, gatifloxacin, etc.) work by inhibiting one or more of a group of enzymes called topoisomerase, enzymes needed for supercoiling, replication, and separation of circular bacterial DNA. For example, DNA gyrase (topoisomerase II) catalyzes the negative supercoiling of the circular DNA found in bacteria. It is critical in bacterial DNA replication, DNA repair, transcription of DNA into RNA, and genetic recombination. Topoisomerase IV, on the other hand, is involved in the relaxation of the supercoiled circular DNA, enabling the separation of the interlinked daughter chromosomes at the end of bacterial DNA replication.
b. Sulfonamides and trimethoprim (synthetic chemicals): Co-trimoxazole is a combination of sulfamethoxazole and trimethoprim. Both of these drugs block enzymes in the bacteria pathway required for the synthesis of tetrahydrofolic acid, a cofactor needed for bacteria to make the nucleotide bases thymine, guanine, uracil, and adenine.
c. Metronidazole is a drug that is activated by the microbial proteins flavodoxin and feredoxin found in microaerophilc and anaerobic bacteria and certain protozoans. Once activated, the metronidazole puts nicks in the microbial DNA strands.
For more information on antibiotics and how they work, see the following CourseArc lesson:
E. MICROBIAL RESISTANCE TO ANTIMICROBIAL CHEMOTHERAPEUTIC AGENTS
A common problem in antimicrobial chemotherapy is the development of resistant strains of bacteria. Most bacteria become resistant to antimicrobial agents by one or more of the following mechanisms:
1. Producing enzymes which inactivate the antibiotic, e.g., penicillinase and other beta-lactamases.
2. Altering the target site in the bacterium to reduce or block binding of the antibiotic, e.g., producing a slightly altered ribosomal subunit that still functions but to which the drug can't bind.
3. Altering the membranes and transport systems to prevent the entry of the antibiotic into the bacterium and/or using an efflux pump to transport the antibiotic out of the bacterium.
4. Developing an alternate metabolic pathway to by-pass the metabolic step being blocked by the antimicrobial agent, e.g., overcoming drugs that resemble substrates and tie-up bacterial enzymes.
5. Increasing the production of a certain bacterial enzyme, e.g., overcoming drugs that resemble substrates and tie-up bacterial enzymes.
These changes in the bacterium that enable it to resist the antimicrobial agent occur naturally because of mutation or genetic recombination of the DNA in the nucleoid, or as a result of obtaining plasmids from other bacteria. Exposure to the antimicrobial agent then selects for these resistant strains of organism.
The spread of antibiotic resistance in pathogenic bacteria is due to both direct selection and indirect selection. Direct selection refers to the selection of antibiotic resistant pathogens at the site of infection. Indirect selection is the selection of antibiotic-resistant normal floras within an individual anytime an antibiotic is given. At a later date, these resistant normal floras may transfer resistance genes to pathogens that enter the body. In addition, these resistant normal flora may be transmitted from person to person through such means as the fecal-oral route or through respiratory secretions.
As an example, many Gram-negative bacteria possess R (resistance) plasmids which have genes coding for multiple antibiotic resistance through the mechanisms stated above, as well as transfer genes coding for a sex pilus. Such an organism can conjugate with other bacteria and transfer an R plasmid to them. Escherichia coli, Proteus, Serratia, Salmonella, Shigella, and Pseudomonas are examples of bacteria which frequently have R plasmids. Because of the problem of antibiotic resistance, antibiotic susceptibility testing is usually done in the clinical laboratory to determine which antimicrobial chemotherapeutic agents will most likely be effective on a particular strain of microorganism. This is discussed in the next section.
To illustrate how plasmids carrying genes coding for antibiotic resistance can be picked up by antibiotic-sensitive bacteria, in today's lab we will use plasmid DNA to transform an Escherichia coli sensitive to the antibiotic ampicillin into one that is resistant to the drug.
The E. coli will be rendered more "competent" to take up plasmid DNA (pAMP), which contains a gene coding for ampicillin resistance, by treating them with a solution of calcium chloride, cold incubation, and a brief heat shock. They will then be plated on 2 types of media: Lauria-Bertani agar (LB) and Lauria-Bertani agar with ampicillin (LB/amp). Only E. coli that have picked up a plasmid coding for ampicillin resistance will be able to form colonies on the LB/amp agar.
For more information on microbial resistance to antibiotics, see the following CourseArc lesson:
F. ANTIBIOTIC SUSCEPTIBILITY TESTING
For some microorganisms, susceptibility to chemotherapeutic agents is predictable. However, for many microorganisms (Pseudomonas, Staphylococcus aureus, and Gram-negative enteric bacilli such as Escherichia coli, Serratia, Proteus, etc.) there is no reliable way of predicting which antimicrobial agent will be effective in a given case. This is especially true with the emergence of many antibiotic-resistant strains of bacteria. Because of this, antibiotic susceptibility testing is often essential to determine which antimicrobial agent to use against a specific strain of bacterium.
Several tests may be used to tell a physician which antimicrobial agent is most likely to combat a specific pathogen:
1. Tube dilution tests
In this test, a series of culture tubes are prepared, each containing a liquid medium and a different concentration of a chemotherapeutic agent. The tubes are then inoculated with the test organism and incubated for 16-20 hours at 35C. After incubation, the tubes are examined for turbidity (growth). The lowest concentration of chemotherapeutic agent capable of preventing growth of the test organism is the minimum inhibitory concentration (MIC).
Subculturing of tubes showing no turbidity into tubes containing medium but no chemotherapeutic agent can determine the minimum bactericidal concentration (MBC). MBC is the lowest concentration of the chemotherapeutic agent that results in no growth (turbidity) of the subcultures. These tests, however, are rather time consuming and expensive to perform.
2. The agar diffusion test (Bauer-Kirby test)
A procedure commonly used in clinical labs to determine antimicrobial susceptibility is the Bauer-Kirby disc diffusion method. In this test, the in vitro response of bacteria to a standardized antibiotic-containing disc has been correlated with the clinical response of patients given that drug.
In the development of this method, a single high-potency disc of each chosen chemotherapeutic agent was used. Zones of growth inhibition (see Fig. 1) surrounding each type of disc were correlated with the minimum inhibitory concentrations of each antimicrobial agent (as determined by the tube dilution test). The MIC for each agent was then compared to the usually-attained blood level in the patient with adequate dosage. Categories of "Resistant," "Intermediate," and "Susceptible" were then established.
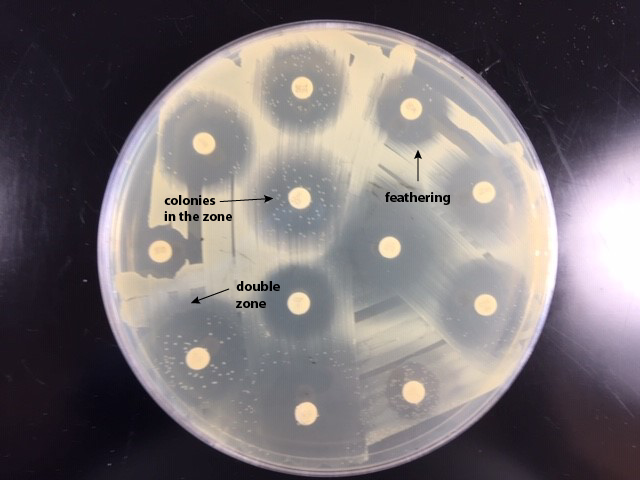
Fig. 1
Antibiotic Susceptibility TestingAntibiotic susceptibility testing plate showing zones of inhibition (arrow) around the antibiotic discs. You measure the diameter of zones of inhibition in millimeters. ; Gary E. Kaiser, Ph.D.
Professor of Microbiology
The Community College of Baltimore County, Catonsville Campus
This work is licensed under a Creative Commons Attribution 3.0 Unported License
The basic steps for the Bauer-Kirby method of antimicrobial susceptibility testing are given below. This outline of procedure is intended to be used as an adjunct to clinical laboratory instruction. The procedure is highly regulated and controlled by the Clinical and Laboratory Standards Institute (CLSI) and must be accompanied by a rigorous quality assurance proGram including performance by certified and/or licensed personnel when the results are to be reported in clinical settings.
a. Prepare a standard turbidity inoculum of the test bacterium so that a certain density of bacteria will be put on the plate.
- Select 3-5 isolated colonies of the bacterium that is being tested.
- If the organism is a Staphylococcus or is fastidious and grows unpredictably in broth like the streptococci, suspend the colonies is saline, Mueller Hinton broth or trypticase soy broth. If the organism grows rapidly in broth, place the colonies in Mueller Hinton broth or trypticase soy broth and incubate 2-8 hours.
- Match the turbidity of the test suspension or culture with a 0.5 McFarland standard. (McFarland standards are tubes containing either latex particles or barium sulfate and adjusted to a standard turbity.)
- If the bacterial suspension is too turbid, add more saline or broth.
- If the bacterial suspension is too light, pick off more colonies and suspend them in the broth or incubate longer.
b. Inoculate a 150mm Mueller-Hinton agar plate with the standardized inoculum so as to cover the entire agar surface with bacteria.
- Dip a sterile swab into the previously standardized tube of the bacterium being tested.Squeeze the swab against the inner wall of the tube to remove excess liquid.
- Swab the entire plate from top to bottom, edge-to-edge leaving no gaps.
- Rotate the plate approximately 60 degrees and using the same swab, again swab the entire plate from top to bottom.
- Rotate the plate approximately 60 degrees and using the same swab, and swab the entire plate from top to bottom a third time.
c. Place standardized antibiotic-containing discs on the plate.
d. Incubate the plate agar side up. For nonfastidious bacteria, incubate at 35°C for 16-18 hours. For fastidious bacteria, follow CLSI standards.
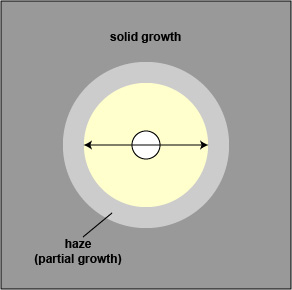
e. Measure the diameter of any resulting zones of inhibition in millimeters (mm) as shown in Fig. 2 .
Fig. 2
Antibiotic Susceptibility Testing
Antibiotic susceptibility testing plate. You measure the diameter of zones of inhibition in millimeters. The zone seen here measures 20 mm in diameter.Gary E. Kaiser, Ph.D.
Professor of Microbiology
The Community College of Baltimore County, Catonsville Campus
This work is licensed under a Creative Commons Attribution 3.0 Unported License
f. Determine if the bacterium is susceptible, moderately susceptible, intermediate, or resistant to each antimicrobial agent using a standardized table (see Table 2). (The latest interpretation tables can be found in CLSI document M100 which is updated every January.)
- If there is a double zone of inhibition, measure the diameter of the innermost zone.
- If there is a zone containing colonies, measure the diameter of the colony free zone.
- If there is a feathered zone, measure the diameter of the point where there is an obvious demarcation between growth and no growth.
- When testing swarming Proteus mirabilis, ignore the swarming.
- When testing Staphylococcus aureus, the haze around an oxacillin should not be ignored. Measure the diameter of the zone free of growth or haze.
The term intermediate generally means that the result is inconclusive for that drug-organism combination. The term moderately susceptible is usually applied to those situations where a drug may be used for infections in a particular body site, e.g., cystitis because the drug becomes highly concentrated in the urine.
3. Automated tests
Computerized automated tests have been developed for antimicrobial susceptibility testing. These tests measure the inhibitory effect of the antimicrobial agents in a liquid medium by using light scattering to determine growth of the test organism. Results can be obtained within a few hours. Labs performing very large numbers of susceptibility tests frequently use the automated methods but the equipment is quite expensive.
PROCEDURES
PROCEDURE FOR MICROBIAL RESISTANCE TO ANTIMICROBIAL CHEMOTHERAPEUTIC AGENTS
MATERIALS
Plasmid DNA (pAMP) on ice, calcium chloride solution on ice, 2 sterile culture tubes, 1 tube of LB broth, 2 plates of LB agar, 2 plates of LB agar with ampicillin (LB/amp), sterile 1 ml transfer pipettes, sterile plastic inoculating loops, bent glass rod, turntable, alcohol, beaker of ice, water bath at 42°C.
ORGANISM
LB agar culture of Escherichia coli
MICROBIAL RESISTANCE PROCEDURE: demonstration
1. Label one LB agar plate "Transformed Bacteria, Positive control" and the other LB agar plate "Wild-Type Bacteria, Positive Control."
Label one LB/amp agar plate "Transformed Bacteria, Experiment" and the other LB/amp agar plate "Wild-Type Bacteria, Negative Control."
2. Label one sterile culture tube "(+) AMP" and the other "(-) AMP." Using a sterile 1ml transfer pipette, add 250 µl of ice cold calcium chloride to each tube. Place both tubes on ice.
Using a sterile plastic inoculating loop, transfer 1-2 large colonies of E. coli into the (+) AMP tube and vigorously tap against the wall of the tube to dislodge all the bacteria. Immediately suspend the cells by repeatedly pipeting in and out with a sterile transfer pipette until no visible clumps of bacteria remain. Return tube to the ice.
3. Repeat step 3 this time using the (-) AMP tube and return to the ice.
4. Using a sterile plastic inoculating loop, add one loopful of pDNA (plasmid DNA) solution to the (+) AMP tube and swish loop to mix the DNA. Return to the ice.
5. Incubate both tubes on ice for 15 minutes.
6. After 15 minutes, "heat-shock" both tube of bacteria by immersing them in a 42°C water bath for 90 seconds. Return both tubes to the ice for 1 minute or more.
7. Using a sterile 1ml transfer pipette, add 250 µl of LB broth to each tube. Tap tubes with your fingers to mix. Set tubes in a test tube rack at room temperature.
8. Using a sterile 1ml transfer pipette, add 100 µl of E. coli suspension from the (-)AMP tube onto the LB/amp agar plate labeled "Wild-Type Bacteria, Negative Control." Add another 100 l of E. coli from the (-)AMP to the LB agar plate labeled "Wild-Type Bacteria, Positive Control."
9. Using a bent glass rod dipped in alcohol and flamed, spread the bacteria thoroughly over both agar plates. Make sure you reflame the glass rod between plates.
10. Using a sterile 1ml transfer pipette, add 100 µl of E. coli suspension from the (+) AMP tube onto the LB/amp agar plate labeled "Transformed Bacteria, Experiment." Add another 100 l of E. coli from the (+) AMP to the LB agar plate labeled "Transformed Bacteria, Positive Control."
11. Immediately spread as in step 10.
12. Incubate all plates at upside down and stacked in the petri plate holder on the shelf of the 37°C incubator corresponding to your lab section until the next lab period.
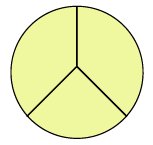
The procedure is summarized in Fig. 3.
Fig. 3
Transfer of Plasmid-Mediated Resistance to Ampicillin in E. coliGary E. Kaiser, Ph.D.
Professor of Microbiology
The Community College of Baltimore County, Catonsville Campus
This work is licensed under a Creative Commons Attribution 3.0 Unported License
PROCEDURE FOR ANTIBIOTIC SUSCEPTIBILITY TESTING
Videos reviewing techniques used in this lab:
Bauer-Kirby Antibiotic Susceptibility Testing Procedure
Interpreting the Results of the Bauer-Kirby Method of Antibiotic Susceptibility Testing
MATERIALS
150mm Mueller-Hinton agar plates (3)
Sterile swabs (3)
An antibiotic disc dispenser containing discs of antibiotics commonly effective against Gram-positive bacteria, and one containing discs of antibiotics commonly effective against Gram-negative bacteria
ORGANISMS
Trypticase Soy broth cultures of Staphylococcus aureus (Gram-positive), Enterococcus faecalis (Gram-positive), and Pseudomonas aeruginosa (Gram-negative)
ANTIBIOTIC SUSCEPTIBILITY TESTING PROCEDURE: to be done in groups of 3
The basic steps for the Bauer-Kirby method of antimicrobial susceptibility testing are given below. This outline of procedure is intended to be used as an adjunct to general microbiology laboratory instruction. The procedure is highly regulated and controlled by the Clinical and Laboratory Standards Institute (CLSI) and must be accompanied by a rigorous quality assurance program including performance by certified and/or licensed personnel when the results are to be reported in clinical settings.
1. Take 3 Mueller-Hinton agar plates. Label one S. aureus, one E. faecalis, and one P. aeruginosa.
2. Using your wax marker, divide each plate into thirds to guide your streaking.
3. Dip a sterile swab into the previously-standardized tube of S. aureus. Squeeze the swab against the inner wall of the tube to remove excess liquid.
4. Streak the swab perpendicular to each of the 3 lines drawn on the plate overlapping the streaks to assure complete coverage of the entire agar surface with inoculum.
5. Repeat steps 3 and 4 for the E. faecalis and P. aeruginosa plates.
6. Using the appropriate antibiotic disc dispenser, place Gram-positive antibiotic-containing discs on the plates of S. aureus and E. faecalis; Gram-negative antibiotic-containing discs on the plate of P. aeruginosa.
7. Incubate the 3 plates upside down and stacked on the shelf of the 35°C incubator corresponding to your lab section until the next lab period.
8. Using a metric ruler, measure the diameter of the zone of inhibition around each disc on each plate in mm by placing the ruler on the bottom of the plate (Fig. 2).
Fig. 2
Antibiotic Susceptibility TestingAntibiotic susceptibility testing plate. You measure the diameter of zones of inhibition in millimeters. The zone seen here measures 20 mm in diameter. Gary E. Kaiser, Ph.D.
Professor of Microbiology
The Community College of Baltimore County, Catonsville Campus
This work is licensed under a Creative Commons Attribution 3.0 Unported License
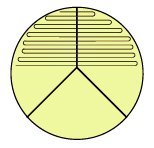
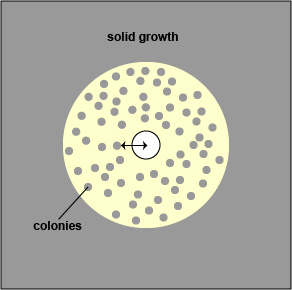
- If there is a double zone of inhibition, measure the diameter of the innermost zone (see Fig. 4A and Fig. 4B).
Fig. 4A:
Double Zone of InhibitionFig. 4B:
Double Zone of Inhibition Colonies in Zone, and FeatheringIf there is a double zone of inhibition, measure the diameter of the innermost zone (arrowed line). Examples of double zone of inhibition, colonies in the zone, and feathering. Gary E. Kaiser, Ph.D.
Professor of Microbiology
The Community College of Baltimore County, Catonsville Campus
This work is licensed under a Creative Commons Attribution 3.0 Unported License
Gary E. Kaiser, Ph.D.
Professor of Microbiology
The Community College of Baltimore County, Catonsville Campus
This work is licensed under a Creative Commons Attribution 3.0 Unported License
- If there is a zone containing colonies, measure the diameter of the colony free zone. Measure from the colony closest to the antibiotic disc to the center of the disc (the radius) and double that number to get the diameter. (See Fig. 5A and Fig. 4B.).
; Fig. 5A:
Zone Containing ColoniesFig. 4B:
Double Zone of Inhibition Colonies in Zone, and FeatheringIf there is a zone containing colonies, measure the diameter of the colony free zone (arrowed line). Examples of double zone of inhibition, colonies in the zone, and feathering. Gary E. Kaiser, Ph.D.
Professor of Microbiology
The Community College of Baltimore County, Catonsville Campus
This work is licensed under a Creative Commons Attribution 3.0 Unported License
Gary E. Kaiser, Ph.D.
;
Professor of Microbiology
The Community College of Baltimore County, Catonsville Campus
This work is licensed under a Creative Commons Attribution 3.0 Unported License
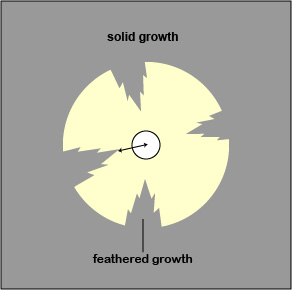
- If there is a feathered zone, measure the diameter of the point where there is an obvious demarcation between growth and no growth. Measure from the end of the feathering closest to the antibiotic disc to the center of the disc (the radius) and double that number to get the diameter. (See Fig. 6A and Fig. 4B).
Fig. 6:
Zone Containing Feathered GrowthFig. 4B:
Double Zone of Inhibition Colonies in Zone, and FeatheringIf there is a zone containing feathered growth, measure the diameter of the growth-free zone (arrowed line). Examples of double zone of inhibition, colonies in the zone, and feathering. Gary E. Kaiser, Ph.D.
Professor of Microbiology
The Community College of Baltimore County, Catonsville Campus
This work is licensed under a Creative Commons Attribution 3.0 Unported License
Gary E. Kaiser, Ph.D.
Professor of Microbiology
The Community College of Baltimore County, Catonsville Campus
This work is licensed under a Creative Commons Attribution 3.0 Unported License
- When testing Staphylococcus aureus, the haze around an oxacillin should not be ignored. Measure the diameter of the zone free of growth or haze.
9. Determine whether each organism is susceptible, moderately susceptible, intermediate, or resistant to each chemotherapeutic agent using the standardized table (Table 2) and record your results.
Table 2
Zone Size Interpretive Chart for Bauer-Kirby Test
Antimicrobial agent Disc code R = mm or less I = mm MS = mm S = mm or more amikacin amoxicillin/
clavulanic acid
- Staphylococcusamoxicillin/
clavulanic acid
- other organismsampicillin
- Staphylococcusampicillin
- G- enterics
Antimicrobial agent Disc code R = mm or less I = mm MS = mm S = mm or more azlocillin aztreonam carbenicillin
- Enterobacteriaceaecarbenicillin
- Pseudomonascefamandole cefazolin
Antimicrobial agent Disc code R = mm or less I = mm MS = mm S = mm or more cefonicid CID-30 14 15-17 - 18 cefoperazone CFP-75 15 - 16-20 21 cefotaxime CTX-30 14 - 15-22 23 cefotetan CTT-30 12 - 13-15 16 cefoxitin FOX-30 13 - 15-17 18 ceftazidime CAZ-30 14 15-17 - 18
Antimicrobial agent Disc code R = mm or less I = mm MS = mm S = mm or more ceftizoxime
- Pseudomonasceftizoxime
- other organismsceftriaxone cefuroxime cephalothin chloramphenicol cinoxacin
Antimicrobial agent Disc code R = mm or less I = mm MS = mm S = mm or more ciprofloxacin clindamycin doxycycline erythromycin gentamicin imipenem kanamycin
Antimicrobial agent Disc code R = mm or less I = mm MS = mm S = mm or more methicillin
- Staphylococcusmezlocillin minocycline moxalactam nafcillin
- Staphylococcusnalidixic acid netilmicin
Antimicrobial agent Disc code R = mm or less I = mm MS = mm S = mm or more nitrofurantoin norfloxacin oxacillin
- Staphylococcuspenicillin Piperacillin/Tazobactum
-Enterobactereaceae
- Staphylococcus or P. aeruginosa
17
17
18-20
-
21
18sulfamethoxazole + trimethoprim
Antimicrobial agent Disc code R = mm or less I = mm MS = mm S = mm or more tetracycline ticarcillin ticarcillin/clavulanic acid tobramycin trimethoprim vancomycin
RESULTS
RESULTS FOR MICROBIAL RESISTANCE TO ANTIMICROBIAL CHEMOTHERAPEUTIC AGENTS
Count the number of colonies on each plate. If the growth is too dense to count individual colonies, record "lawn" (bacteria cover nearly the entire agar surface).
Plate Number of colonies Conclusion LB/amp
"Transformed Bacteria,
Experiment"LB
"Transformed Bacteria,
Positive Control"LB/amp
"Wild-Type Bacteria,
Negative Control"LB
"Wild-Type Bacteria,
Positive Control"
RESULTS FOR ANTIBIOTIC SUSCEPTIBILITY TESTING: BAUER-KIRBY METHOD
Interpret the results following steps 9 and 10 of the procedure and record your results in the tables below.
Staphylococcus aureus
Disc code Antimicrobial agent Zone in mm R I MS S AMC-30 amoxicillin/
clavulanic acidCTX-30 cefotaxime FOX-30 cefoxitin CIP-5 ciprofloxacin DA-2 clindamycin E-15 erythromycin K-30 kanamycin OX-1 oxacillin SXT-25 sulfamethoxazole
+ trimethoprimTE-30 tetracycline TZP110 piperacillin/tazobactum VA-30 vancomycin R = Resistant
I = Intermediate
MS = Moderately Susceptible
S = Susceptible
Enterococcus faecalis
Disc code Antimicrobial agent Zone in mm R I MS S AMC-30 amoxicillin/
clavulanic acidCTX-30 cefotaxime FOX-30 cefoxitin CIP-5 ciprofloxacin DA-2 clindamycin E-15 erythromycin K-30 kanamycin OX-1 oxacillin SXT-25 sulfamethoxazole
+ trimethoprimTE-30 tetracycline TZP-110 piperacillin/tazobactum VA-30 vancomycin R = Resistant
I = Intermediate
MS = Moderately Susceptible
S = Susceptible
Pseudomonas aeruginosa
disc code antimicrobial agent zone in mm R I MS S AK-30 amikacin AMC-30 amoxicillin/
clavulanic acidAMP-10 ampicillin MEZ-75 mezlocillin CTX-30 cefotaxime FOX-30 cefoxitin CIP-5 ciprofloxacin CN-10 gentamicin K-30 kanamycin SXT-25 sulfamethoxazole
+ trimethoprimTE-30 tetracycline TZP-110 piperacillin/tazobactum R = Resistant
I = Intermediate
MS = Moderately Susceptible
S = Susceptible
PERFORMANCE OBJECTIVES FOR LAB 18
After completing this lab, the student will be able to perform the following objectives:
A. DISINFECTANTS, ANTISEPTICS, AND SANITIZERS
1. Define the following terms: sterilization, disinfection, decontamination, disinfectant, antiseptic, and sanitizer.
2. State why chemical agents are usually unreliable for sterilization.
3. List five factors that may influence the antimicrobial action of disinfectants, antiseptics, and sanitizers.
4. Describe two modes of action of disinfectants, antiseptics, and sanitizers, i.e., how they harm the microorganisms.
5. Name two chemical agents that are reliable for sterilization.
B. EVALUATION OF DISINFECTANTS, ANTISEPTICS, AND SANITIZERS
1. State why the results of an in vitro test to evaluate chemical agents may not necessarily apply to in vivo situations.
C. EVALUATION OF HAND WASHING1. Define transient flora and resident flora and compare the two groups in terms of ease of removal.
D. ANTIMICROBIAL CHEMOTHERAPEUTIC AGENTS
1. Define the following: antibiotic, antimicrobial chemotherapeutic chemical, narrow-spectrum antibiotic, broad-spectrum antibiotic.
2. Discuss the meaning of selective toxicity in terms of antimicrobial chemotherapy.
3. List four genera of microorganisms that produce useful antibiotics.
4. Describe four different major modes of action of antimicrobial chemotherapeutic chemicals and give three examples of drugs fitting each mode of action.
E. MICROBIAL RESISTANCE TO ANTIMICROBIAL AGENTS
DISCUSSION
1. State five mechanisms by which microorganisms may resist antimicrobial chemotherapeutic agents.
2. Briefly describe R-plasmids and name four bacteria that commonly possess these plasmids.
RESULTS
1. Interpret the results of the Escherichia coli plasmid transformation experiment.
F. ANTIBIOTIC SUSCEPTIBILITY TESTING
DISCUSSION
1. State why antimicrobial susceptibility testing is often essential in choosing the proper chemotherapeutic agent to use in treating an infection.
2. State what is meant by MIC.
RESULTS
1. Interpret the results of a Bauer-Kirby antimicrobial susceptibility test when given a Mueller-Hinton agar plate, a metric ruler, and a standardized zone-size interpretation table.
SELF-QUIZ
Microbiology Laboratory Manual by Gary E. Kaiser, PhD, Professor of Microbiology
is licensed under a Creative Commons Attribution 4.0 International License.
Last updated: August, 2023